A dose of psilocybin, a dash of rabies point to treatment for depression. Psilocybin, which is the active ingredient in magic mushrooms. Were used ritualistically in pre Columbian Mexico
Psilocybin mushrooms were used ritualistically in pre-Columbian Mexico, but claims of their widespread ancient use are largely exaggerated and shaped by modern idealization and ideology.[28] In 1958, the Swiss chemist Albert Hofmann isolated psilocybin and psilocin from the mushroom Psilocybe mexicana. His employer, Sandoz, marketed and sold pure psilocybin to physicians and clinicians worldwide for use in psychedelic therapy. Increasingly restrictive drug laws of the 1960s and the 1970s curbed scientific research into the effects of psilocybin and other hallucinogens, but its popularity as an entheogen grew in the next decade, owing largely to the increased availability of information on how to cultivate psilocybin mushrooms.
Albert Hofmann isolated psilocybin 1958
An international collaboration led by Cornell researchers used a combination of psilocybin and the rabies virus to map how and where – the psychedelic compound rewires the connections in the brain.
Specifically, they showed psilocybin weakens the cortico-cortical feedback loops that can lock people into negative thinking. Psilocybin also strengthens pathways to subcortical regions that turn sensory perceptions into action, essentially enhancing sensory-motor responses.
The findings published Dec. 5 in Cell. The lead author is postdoctoral researcher Quan Jiang.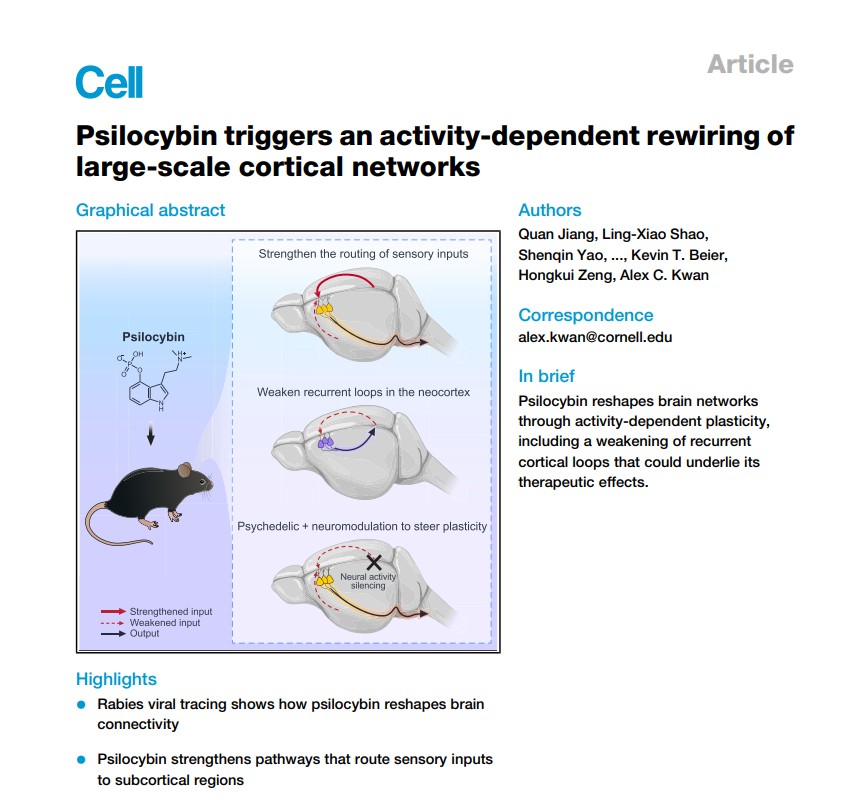
The findings published Dec. 5 in Cell.
The project is the latest in a trail of discoveries led by Alex Kwan, Ph.D. ’09, professor of biomedical engineering in Cornell Engineering and the paper’s senior author.
Kwan’s lab studies the ways psychiatric drugs such as psilocybin, ketamine and 5-MeO-DMT rewire the brain’s neurological circuitry, with the goal of developing therapeutic treatments for depression.
Psilocybin, which is the active ingredient in magic mushrooms, is a promising candidate for pharmaceutical development because the clinical trials have shown that the psychedelic drug can reduce symptoms in people with depression – for weeks and perhaps even months after a single treatment.
In 2021, Kwan’s group used high-resolution optical imaging to show that a single dose of psilocybin induces structural plasticity – the brain’s ability to reshape its structure – by rapidly growing dendritic spines that lead to synaptic connections.
“A lot of people were excited about the earlier study, because psychedelics are promising therapeutics but we don’t know why they work. Our study showed that the rewiring in the brain lasts a long time,” Kwan said. “One of the key questions was that, even though we show that new connections are being made, we don’t know where they connect. The goal of this study is to figure out: what exactly are the parts of the circuit that get rewired?”
To do that, Kwan’s group took a new approach. Instead of using optics to image individual synaptic connections, they paired the psilocybin with one of biology’s wiliest adversaries: the rabies virus. The virus, created by collaborators at the Allen Institute for Brain Science in Seattle, would move through and chart the brain’s “very complex wiring diagram,” Kwan said, much like Google’s mapping cars roaming all the streets in a neighborhood.
“With psilocybin, it’s like we’re adding all these roads to the brain, but we don’t know where the roads go,” Kwan said. “Here we use the rabies virus to read out the connectivity in the brain, because these viruses are engineered in nature to transmit between neurons. That’s how they’re so deadly. It jumps a synapse and goes from one neuron to another.”
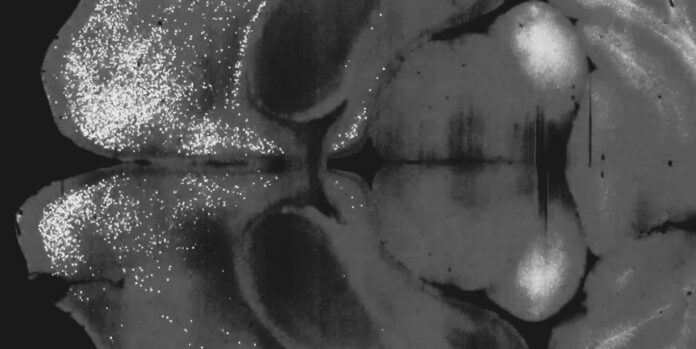
First the researchers injected a single dose of psilocybin into a mouse’s frontal cortical pyramidal neurons. Then a day later, they chased it with a variant of the rabies virus that could transmit across a synapse and label those connected neurons with fluorescent proteins. After the virus had incubated in the mouse for a week, the team imaged its brain and compared the results with a control mouse brain that had only received the virus.
The fluorescent tagging revealed that psilocybin had weakened recurrent connections within the cortex – feedback loops that may explain why a depressed person fixates on negative thoughts.
“Rumination is one of the main points for depression, where people have this unhealthy focus and they keep dwelling on the same negative thoughts,” Kwan said. “By reducing some of these feedback loops, our findings are consistent with the interpretation that psilocybin may rewire the brain to break, or at least weaken, that cycle.”
The researchers also saw that the sensory area of the brain becomes more strongly wired to the subcortical region, strengthening the link between perception and action.
Initially Kwan expected to find connections between one or two regions of the brain, but he was surprised to discover psilocybin’s rewiring involved the whole brain.
“This is really looking at brain-wide changes,” he said. “That’s a scale that we have not worked at before. A lot of times, we’re focusing on a small part of the neural circuit.”
The extensive pathway mapping also showed that the amount of firing activity in the brain may determine what gets rewired by the drug. That inspired the researchers to demonstrate that by perturbing and manipulating the neural activity of one brain region, they could actually change the way psilocybin rewires the circuitry.
“That opens up many possibilities for therapeutics, how you maybe avoid some of the plasticity that’s negative and then enhance specifically those that are positive,” Kwan said.
Co-authors include postdoctoral researcher Ling-Xiao Shao; doctoral student Amelia D. Gilbert; Jack Nothnagel ’25; Neil Savalia and Pasha Davoudian of Yale University; Shenqin Yao and Hongkui Zeng of the Allen Institute for Brain Science in Seattle; Guilian Tian and Kevin Beier of University of California, Irvine; and Tin Shing Hung and Hei Ming Lai of the Chinese University of Hong Kong.
The research was supported by One Mind and the National Institutes of Health.